The Mysterious Eosinophils and Eusinophil Control in Asthma
Asthma is becoming a global epidemic. According to the World Health Organisation, this incurable disease affects around 339 million people and claims around 1,000 lives every day.
Half of asthma patients develop eosinophilic airway inflammation. Eosinophils are part of the immune system. Their primary function is to protect the body from multicellular parasites and the infections they cause. Nonetheless, asthma and some other inflammatory diseases lead to an increase in the number of eosinophils that are characterised by other functions.
These cells migrate into the airways and have a negative impact on the course of the disease, and may sometimes even lead to very severe forms of asthma.
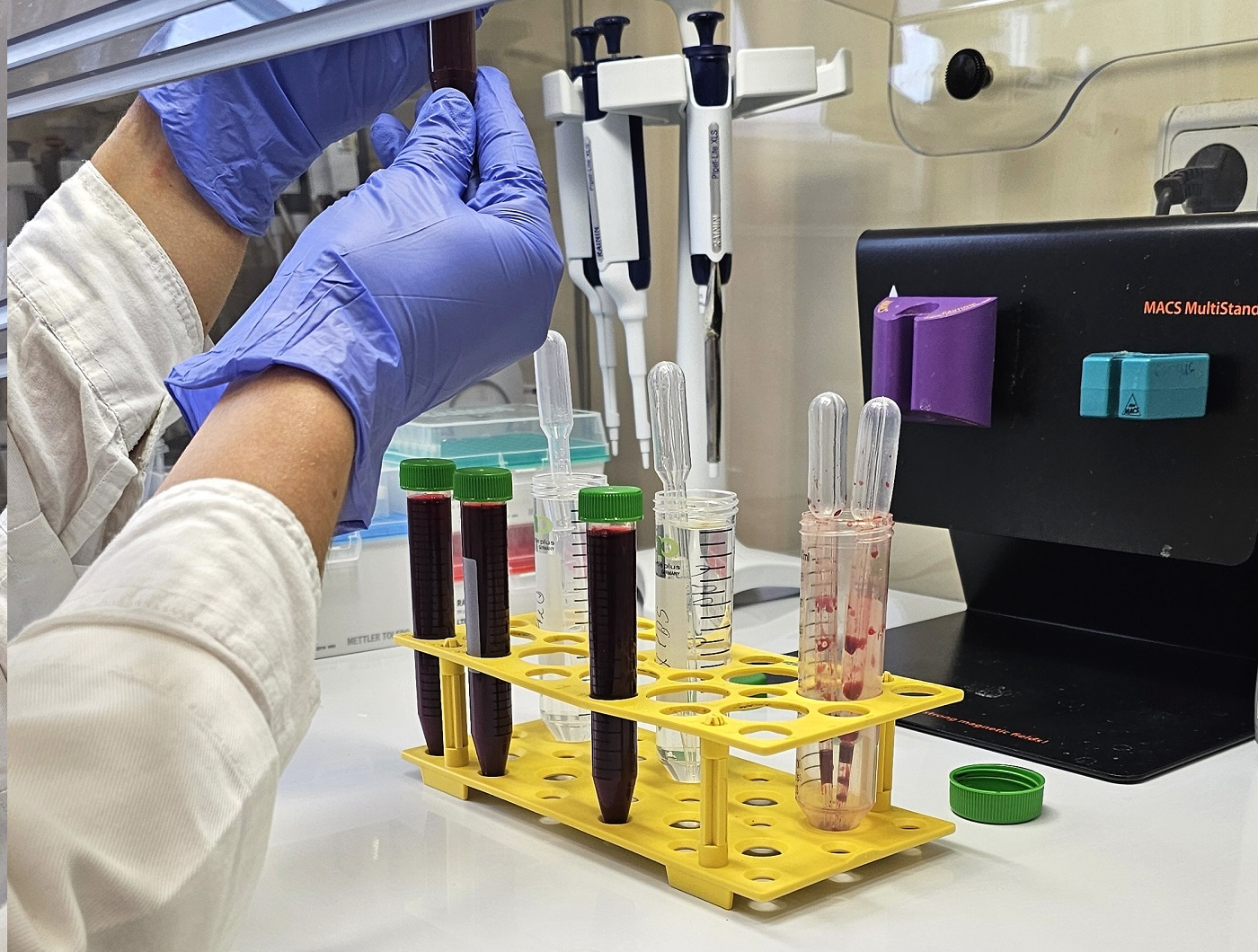
A research team from the Clinical Department of Pulmonology and the Pulmonology Laboratory at the Lithuanian University of Health Sciences (LSMU) has focused its efforts on the study eosinophils, which have been found to behave abnormally in the case of asthma, and even to cause damage to the airways and the lungs. This study is also special because it looks at cells isolated from the blood of people with asthma.
Why do the cells that make up the human immune system start acting in a detrimental way, and how can their negative effects be counteracted?
The “misguided” cells and their different functions
According to Prof. Kęstutis Malakauskas, Head of the Pulmonology Laboratory at the Clinical Department of Pulmonology under the LSMU Medical Academy, eosinophils are not just inflammatory cells. They are involved in specific changes in the state of tissues or organs, and the respiratory tract is no exception.
In the airways, eusinophils act beneficially by ensuring an uninterrupted airway modeling stage. However, in asthma, eosinophils disrupt the intercellular balance in the lungs, causing an unfavourable process of airway remodeling: bronchial smooth muscle mass increases, the airway wall becomes thicker, connective tissue progresses, etc.

Eight years ago, eosinophil subtypes – inflammatory and lung-resident– having different biological properties, were identified for the first time in the world. Inflammatory eosinophils are actively involved in inflammation, while lung-resident eosinophils maintain the balance of lung tissues. Although it is possible to simply refer to them as “good” and “bad”, the quantitative factor is also important, since too many “good” eosinophils also upset the established balance.
These discoveries have opened a new window into the study of eosinophils as a heterogeneous population of cells, and our research team has focused on assessing the biological properties of eosinophil subtypes.
Suppressing the harmful activity
One of the major efforts in recent years have been focused on the study of the effect of eosinophil subtypes on lung structural cells such as bronchial smooth muscle cells and lung fibroblasts. The study was carried out in a combined culture in vitro model, assessing eosinophils isolated from individuals with different asthma phenotypes.
According to Prof. Skaidrius Miliauskas, Head of the Clinical Department of Pulmonology, by inhibiting the influence of certain established factors on eosinophils, it might be possible to control their activity in asthma. However, it remains to be seen whether all factors have the same effect on different subtypes.
“The study has shown that eosinophil subtypes may contribute to structural changes in the airways by promoting migration and division of other cells. Unexpectedly, the strongest effect on these processes was observed in the lung-resident, or “good”, eosinophils, particularly in severe, uncontrolled asthma.
A separate step in this study was the search for different types of asthma-specific biomarkers associated with eosinophilic inflammation. Reliable asthma biomarkers are few and not specific to a particular asthma phenotype.
By enrolling allergic and non-allergic asthma patients, we compared the blood levels of selected markers and identified 5 newly discovered biologically active substances that could be used as potential biomarkers of allergic asthma phenotype. We also investigated changes in the expression of micro ribonucleic acids (miRNAs) related to eosinophil subtypes, their effect on target genes, and their blood levels,” said Prof. S. Miliauskas.
“This is a unique opportunity to work with eosinophils, and we are very grateful to those who agreed to take part in the study. Until now, biological research has largely been carried out using animal models of asthma.
The main unique feature of our study is the use of a combined cell culture model, which enables direct contact between eosinophils isolated from the subjects’ blood with in vitro cultured airway structural cells, such as bronchial smooth muscle cells and lung fibroblasts.
Eosinophils are the cells that secrete extremely high levels of different cytokines, chemokines, growth factors, and enzymes. The importance of all these factors in asthma is unquestionable, but there are no studies assessing the direct effect of eosinophils on other cells after attachment to their surface.
Using this method, we can answer more precisely which processes eosinophils are directly involved in, and even where they act only as mediators, whether or not they need feedback, or additional activation from other cells”, – said Dr. Andrius Januškevičius, researcher at the Pulmonology Laboratory of the Clinical Department of Pulmonology under the LSMU Medical Academy.
Research will continue
Eosinophil research is ongoing and results are published in open-access scientific journals. Further research on the biological properties of eosinophils is planned to include new structural cells such as epithelial cells.

Part of the research was carried out by LSMU researchers in collaboration with researchers from the Human Genome Research Group of Vilnius University, Dr. Kristina Šnipaitiene and PhD student Benita Buragaite, under the supervision of the group leader Prof. Dr. Sonata Jarmalaite.
The research team of the Clinical Department of Pulmonology and Pulmonology Laboratory under the LSMU Medical Academy included Prof. Dr. Kęstutis Malakauskas (Head of the Laboratory) Prof. Dr. Skaidrius Miliauskas (Head of the Clinical Department), Dr. Andrius Januškevičius, Assoc. Prof. Dr. Virginija Kalinauskaite-Zukauskas, doctor Jolita Palačionytė, PhD student Eglė Vasylė, and PhD student Airidas Rimkūnas.
Studies of eosinophil activity and effects on other cells contribute to a more detailed understanding of the biological properties of eosinophils and lay the groundwork for possible strategies to inhibit individual eosinophil functions in asthma.
